Introduction
Obsessive–compulsive disorder (OCD) is often misunderstood. Casual phrases like “I’m so OCD” are commonly used to describe neatness or a preference for order, but these everyday jokes distort the reality of a serious mental health condition. It is a chronic psychiatric disorder characterized by intrusive, unwanted thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to reduce distress. For many individuals, it consumes hours each day and significantly interferes with work, relationships, and quality of life (American Psychiatric Association [APA], 2022).
Read More: Sleep and Mental Health
Myth 1: OCD is just being neat or a perfectionist
Reality: OCD is driven by anxiety and intrusive thoughts, not preference.
Perfectionism and tidiness are personality traits. It, however, involves ego-dystonic thoughts—ideas that feel unwanted, distressing, and inconsistent with the person’s values. Compulsions are not performed for satisfaction or pleasure, but to neutralize fear or anxiety. Someone with Obsessive–compulsive disorder may repeatedly check locks not because they enjoy certainty, but because they are tormented by the fear of catastrophic consequences if they do not (Abramowitz et al., 2009).
Myth 2: Everyone is “a little OCD”
Reality: OCD is a diagnosable disorder with specific criteria.
According to diagnostic standards, OCD requires obsessions and/or compulsions that are time-consuming (typically more than one hour per day) or cause clinically significant distress or impairment (APA, 2022). While many people prefer order, this does not equate to Obsessive–compulsive disorder. Suggesting that “everyone has OCD” minimizes the severity of the disorder and discourages individuals from seeking treatment.
Myth 3: People with OCD could stop their behaviors if they tried
Reality: Compulsions are reinforced by anxiety reduction.

Compulsions temporarily reduce anxiety, reinforcing the behavior through negative reinforcement. This learning cycle makes stopping rituals extremely difficult without professional help. Cognitive behavioral therapy (CBT) with exposure and response prevention (ERP) is designed to break this cycle by gradually exposing individuals to feared situations while preventing compulsive responses (Foa et al., 2012).
Myth 4: OCD is caused by bad parenting or weak character
Reality: OCD has biological, genetic, and environmental contributors.
Research shows that it has a significant genetic component, with heritability estimates ranging from 40–50% (Pauls et al., 2014). Neuroimaging studies implicate dysfunction in cortico-striato-thalamo-cortical circuits. Stressful life events can exacerbate symptoms, but OCD is not caused by poor parenting or moral weakness.
Myth 5: Medication is the only effective treatment
Reality: Psychotherapy and medication are both evidence-based.
The most effective treatments for obsessive–compulsive disorder are CBT with ERP and selective serotonin reuptake inhibitors (SSRIs). Many individuals benefit from psychotherapy alone, while others respond best to a combination of therapy and medication (NICE, 2020). Treatment choice depends on symptom severity, comorbidities, and patient preference.
Myth 6: OCD always involves visible rituals
Reality: Mental compulsions are common.
Some individuals perform compulsions internally, such as counting, praying silently, or mentally reviewing events. These covert rituals are harder to detect and often misunderstood, leading to underdiagnosis or mislabeling as generalized anxiety or rumination (Abramowitz et al., 2009).
Myth 7: OCD is only about germs and cleaning
Reality: Obsessive–compulsive disorder has many symptom dimensions.
Obsessive–compulsive disorder can involve checking, symmetry, intrusive taboo thoughts, reassurance-seeking, and hoarding-related behaviors. Intrusive thoughts may involve violence, sexuality, or religion, which are particularly distressing due to shame and fear of judgment. Importantly, these thoughts do not indicate intent to act (APA, 2022).
Evidence-Based Treatment Overview
CBT with ERP:
ERP is considered the gold standard psychological treatment for OCD and has strong empirical support across age groups (Foa et al., 2012).
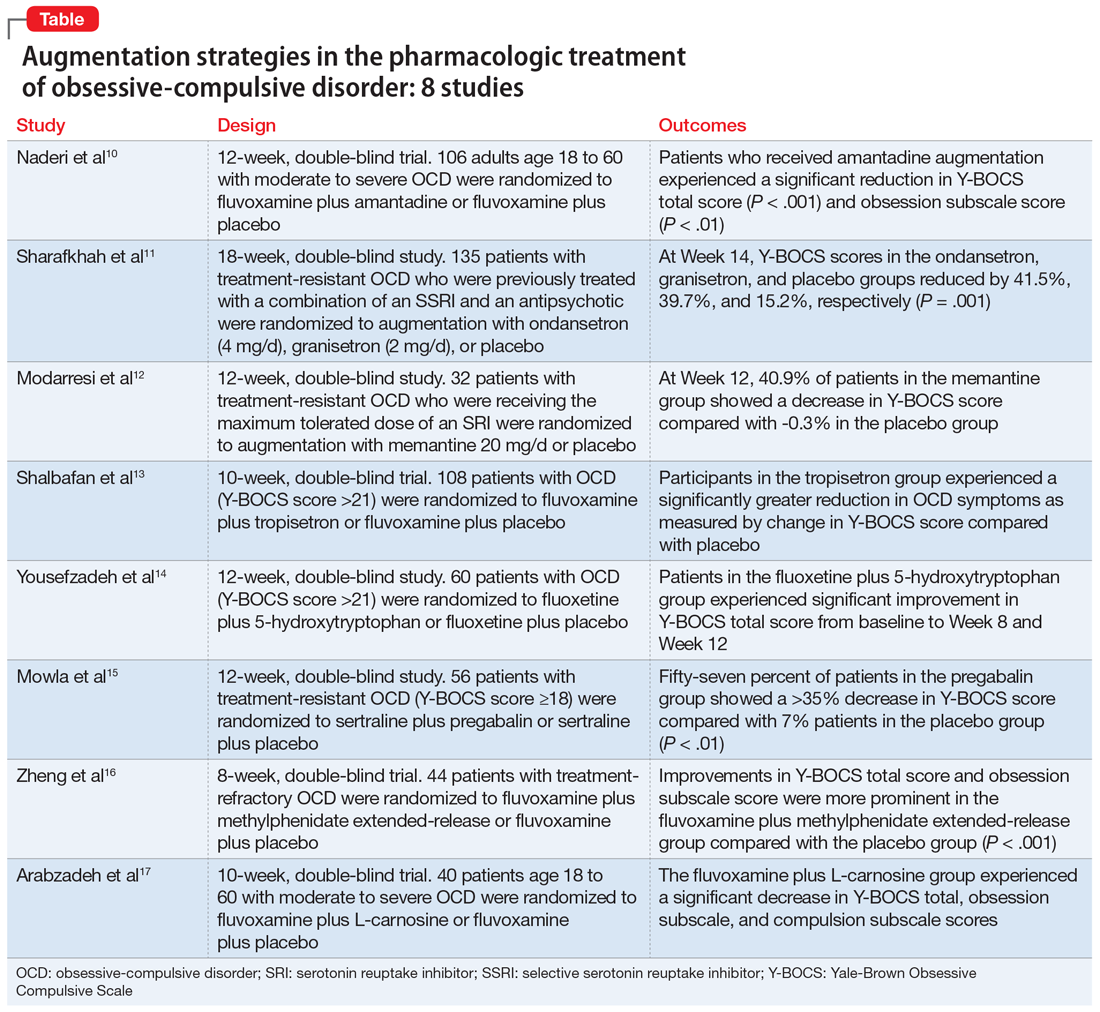
Pharmacotherapy:
SSRIs and clomipramine have demonstrated efficacy, often at higher doses than those used for depression (Stein et al., 2019).
Combined treatment:
For moderate to severe OCD, combining medication with ERP often yields the best outcomes (NICE, 2020).
Conclusion
It is a serious, multifaceted mental health disorder—not a personality quirk. Dispelling myths about it promotes understanding, reduces stigma, and helps individuals access effective treatment. With appropriate care, many people with it experience significant symptom reduction and improved quality of life.
References
Abramowitz, J. S., Taylor, S., & McKay, D. (2009). Obsessive–compulsive disorder. The Lancet, 374(9688), 491–499.
American Psychiatric Association. (2022). DSM-5-TR: Diagnostic and statistical manual of mental disorders (5th ed., text rev.).
Foa, E. B., Yadin, E., & Lichner, T. K. (2012). Exposure and response prevention for OCD: Therapist guide. Oxford University Press.
National Institute for Health and Care Excellence. (2020). Obsessive-compulsive disorder and body dysmorphic disorder: Treatment.
Pauls, D. L., Abramovitch, A., Rauch, S. L., & Geller, D. A. (2014). Obsessive–compulsive disorder: An integrative genetic and neurobiological perspective. Nature Reviews Neuroscience, 15(6), 410–424.
Stein, D. J., Costa, D. L. C., Lochner, C., Miguel, E. C., Reddy, Y. C. J., Shavitt, R. G., … Simpson, H. B. (2019). Obsessive–compulsive disorder. Nature Reviews Disease Primers, 5(52).
Subscribe to PsychUniverse
Get the latest updates and insights.
Join 3,036 other subscribers!
Niwlikar, B. A. (2025, December 20). 7 Important OCD Myths vs. Psychological Reality. PsychUniverse. https://psychuniverse.com/ocd-myths/



