Introduction
In recent years, scientific research has uncovered a fascinating link between gut health and mental well-being, known as the gut-brain axis. This emerging field of study suggests that the trillions of microorganisms residing in the gut—collectively known as the gut microbiome—play a crucial role in regulating mood, cognition, and mental health. From depression and anxiety to neurodegenerative diseases, the gut microbiome’s influence extends far beyond digestion.
Read More- Mental Health and Ways to Improve It
Understanding the Gut-Brain Axis
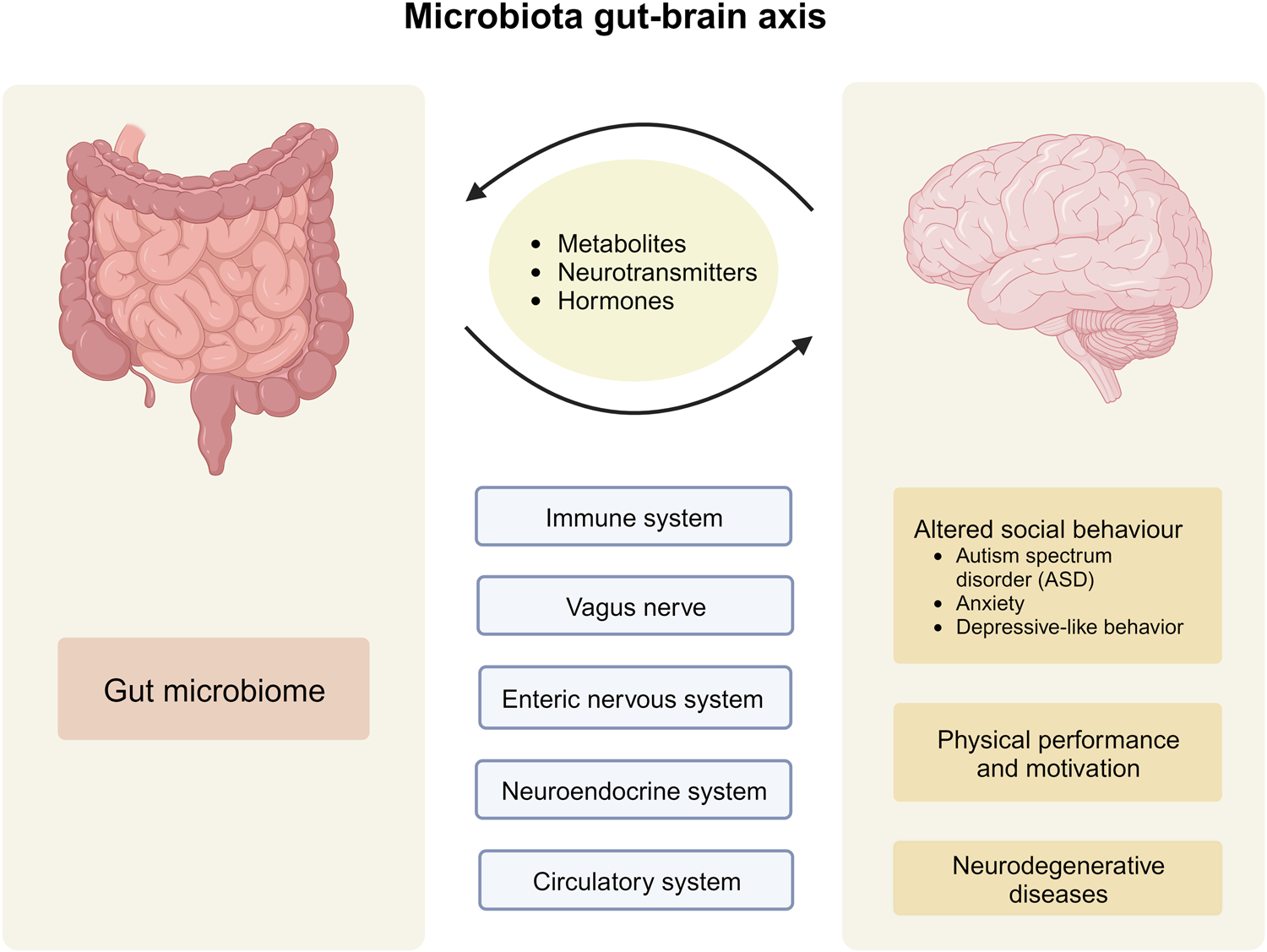
The gut-brain axis is a bidirectional communication network linking the gastrointestinal tract and the central nervous system (CNS). This complex interaction occurs through various pathways, including the vagus nerve, the immune system, and gut-derived neurotransmitters (Cryan & Dinan, 2012). Researchers have discovered that gut bacteria influence brain function by producing neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA), which play essential roles in regulating emotions and cognitive processes (Carabotti et al., 2015).
Role of Gut Microbiota in Mental Health
Role of gut microbiota in mental health can be understood in terms of-
1. Depression and Anxiety
Studies have shown that individuals with mood disorders often exhibit dysbiosis, an imbalance in gut microbiota composition (Foster & McVey Neufeld, 2013). Certain beneficial bacteria, such as Lactobacillus and Bifidobacterium, help produce serotonin, the neurotransmitter responsible for regulating mood and well-being. A disrupted gut microbiome can lead to decreased serotonin production, contributing to symptoms of depression and anxiety (Clarke et al., 2013).
2. Stress and Cortisol Regulation
The gut microbiome influences the body’s stress response via the hypothalamic-pituitary-adrenal (HPA) axis. Chronic stress can alter gut microbiota composition, leading to increased cortisol levels, which negatively affect brain function and emotional regulation (Dinan & Cryan, 2017). Research suggests that probiotics, or “good” bacteria, can help modulate the stress response by restoring microbial balance (Ait-Belgnaoui et al., 2012).
3. Neurodevelopmental and Neurodegenerative Disorders
Emerging evidence suggests that gut microbiota play a role in conditions like autism spectrum disorder (ASD), Alzheimer’s disease, and Parkinson’s disease. Studies on ASD have found altered gut microbiomes in affected individuals, suggesting a potential link between gut bacteria and neurodevelopment (Krajmalnik-Brown et al., 2015). Similarly, research on Alzheimer’s and Parkinson’s diseases indicates that gut inflammation and microbiome dysbiosis may contribute to neurodegeneration (Scheperjans et al., 2015).
Mechanisms of the Gut-Brain Connection
The mechanism on which the gut brain connection works includes-
1. Neurotransmitter Production
Gut bacteria produce neurotransmitters that influence brain function. For example:
- Serotonin: About 90% of the body’s serotonin is produced in the gut, regulating mood and anxiety (Yano et al., 2015).
- Dopamine: Influences motivation and pleasure; gut microbes contribute to its synthesis (Mittal et al., 2017).
- GABA: Helps reduce stress and anxiety, and certain gut bacteria enhance its production (Patterson et al., 2019).
2. Immune System Modulation
The gut microbiome plays a vital role in immune function, influencing brain health through inflammation control. Chronic gut inflammation has been linked to mental health disorders, including depression and schizophrenia (Miller & Raison, 2016).
3. The Vagus Nerve Pathway
The vagus nerve serves as a communication highway between the gut and brain. Research suggests that stimulating the vagus nerve through gut health improvements can positively affect mood and cognitive function (Bonaz et al., 2018).

Strategies for Enhancing Mental Health Through Gut Health
Some ways to enhance mental health through the gut health include-
1. Probiotics and Prebiotics
Probiotics (live beneficial bacteria) and prebiotics (fibers that feed good bacteria) have shown promise in improving mood and reducing anxiety. Studies suggest that probiotic supplementation can help restore gut balance and enhance emotional well-being (Messaoudi et al., 2011).
2. Diet and Nutrition
A diet rich in fiber, fermented foods, and omega-3 fatty acids supports a healthy gut microbiome. The Mediterranean diet, which includes fruits, vegetables, nuts, and fermented foods, has been linked to lower rates of depression and anxiety (Jacka et al., 2017).
3. Stress Management and Exercise
Regular physical activity and mindfulness practices like meditation positively impact gut health by reducing stress and promoting microbial diversity (Patterson et al., 2019).

Conclusion
The gut-brain connection is a groundbreaking area of research with profound implications for mental health. By understanding how gut microbiota influence mood, stress response, and neurodevelopment, we can develop targeted interventions to improve mental well-being. Future research will continue to uncover new ways to harness the power of the microbiome for psychological health, offering hope for innovative treatments in psychiatry and neurology.
References
Ait-Belgnaoui, A., Durand, H., Cartier, C., et al. (2012). Prevention of gut leakiness by a probiotic treatment leads to attenuated HPA response to an acute psychological stress in rats. Psychoneuroendocrinology, 37(11), 1885-1895.
Bonaz, B., Bazin, T., & Pellissier, S. (2018). The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in Neuroscience, 12, 49.
Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology, 28(2), 203-209.
Clarke, G., Grenham, S., Scully, P., et al. (2013). The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Molecular Psychiatry, 18(6), 666-673.
Cryan, J. F., & Dinan, T. G. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behavior. Nature Reviews Neuroscience, 13(10), 701-712.
Dinan, T. G., & Cryan, J. F. (2017). Gut instincts: microbiota as a key regulator of brain development, ageing and neurodegeneration. The Journal of Physiology, 595(2), 489-503.
Foster, J. A., & McVey Neufeld, K. A. (2013). Gut-brain axis: how the microbiome influences anxiety and depression. Trends in Neurosciences, 36(5), 305-312.
Jacka, F. N., O’Neil, A., Opie, R., et al. (2017). A randomised controlled trial of dietary improvement for adults with major depression (“SMILES”). BMC Medicine, 15(1), 23.
Scheperjans, F., Aho, V., Pereira, P. A. B., et al. (2015). Gut microbiota are related to Parkinson’s disease and clinical phenotype. Movement Disorders, 30(3), 350-358.
Yano, J. M., Yu, K., Donaldson, G. P., et al. (2015). Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell, 161(2), 264-276.
Subscribe to PsychUniverse
Get the latest updates and insights.
Join 3,043 other subscribers!
Niwlikar, B. A. (2025, March 18). Gut-Brain Axis and Its 3 Important Roles in Mental Health. PsychUniverse. https://psychuniverse.com/gut-brain-axis/




